Since humans first learned to harness these substances from plants, drug addiction, or the excessive use of narcotics like cocaine, has been linked to psychological degeneration and general health decline.
Cocaine, opioids, and other abused substances damage the brain’s reward system, causing users to prioritize getting more drugs over everything else. This persistent urge is notoriously tough to overcome for those struggling with addiction, but new research from MIT’s McGovern Institute for Brain Research and partners suggests a therapy technique that might assist.
The new study shows how drugs inhibit or alter the brain’s reward system, which, when activated, allows us to experience pleasure and pleasant emotions. As a result, blocking this mechanism permits drugs to shift our perceived benefits away from other sources of rewards and toward additional drugs.
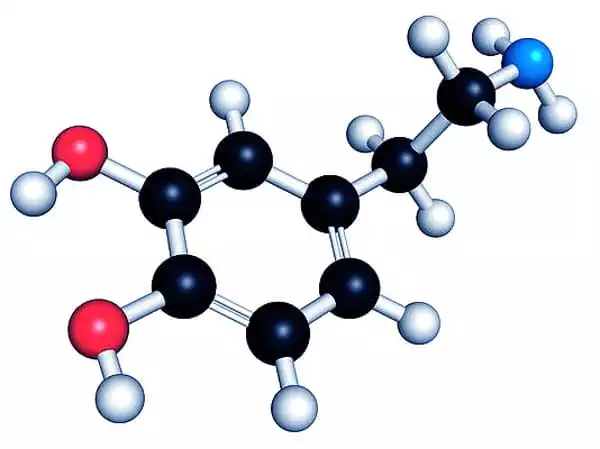
In a Jan. 25 online publication in the journal Addiction Biology, researchers from MIT Institute Professor Ann Graybiel’s lab and collaborators from the University of Copenhagen and Vanderbilt University report that activating a signaling molecule in the brain known as muscarinic receptor 4 (M4) causes rodents to reduce cocaine self-administration while simultaneously choosing a food treat over cocaine.
M4 receptors can be located on the surface of neurons in the brain, where they change signaling in response to the neurotransmitter acetylcholine. They are abundant in the striatum, a brain area implicated in habit development by Graybiel’s group. Addiction researchers are interested in them because, together with a similar receptor called M1, which is also widespread in the striatum, they frequently appear to work in opposition to the neurotransmitter dopamine.
Drugs of abuse excite the habit circuits of the brain by enabling dopamine to accumulate in the brain. Chronic usage can cause that circuitry to become less sensitive to dopamine, making previously rewarding events less enjoyable and driving users to seek bigger amounts of their substance. Attempts to inhibit the dopamine system directly have not been proven to be useful in treating addiction and can have unpleasant or severe side effects, therefore researchers are looking for an alternate technique to restore balance within the brain’s reward circuitry. “Activating these muscarinic receptors is another approach to adjust that system,” says Jill Crittenden, a research scientist in the Graybiel lab.
Morgane Thomsen, a neuroscientist at the University of Copenhagen, discovered that stimulating the M1 receptor caused mice to choose food over cocaine. In the latest study, she demonstrated that a medication that specifically stimulates the M4 receptor had a comparable impact. When rats who have been trained to self-administer cocaine are given an M4-activating chemical, they instantly reduce their drug usage and aggressively choose food instead. Thomsen discovered that this impact increased greater during a seven-day course of therapy, with cocaine consumption decreasing day by day. When the M4-activating medication was withdrawn, the rats soon recovered their previous cocaine-seeking behavior.
While Thomsen’s research have now proven that activating either M1 or M4 will lower animal cocaine usage, it is obvious that the two muscarinic receptors do not influence cocaine use in the same way. M1 activation operates on a distinct time scale, taking some time to kick in yet leaving some effects long after the therapy is stopped.
Graybiel’s lab has confirmed that the two receptors impact drug-seeking behavior via separate biochemical pathways in genetically engineered mice. Previously, the researchers observed that activating M1 had no effect on cocaine desire in mice lacking the CalDAG-GEFI signaling protein. M4 activation, on the other hand, lowers cocaine intake independent of the presence of CalDAG-GEFI.
“The CalDAG-GEFI is entirely necessary for the M1 impact to occur, but it does not appear to play any part in the M4 effect”
Thomsen
The findings imply that activating M4 might aid in the recovery of patients suffering from drug misuse problems and that this method could be even more beneficial if paired with M1 receptor activation.
When Graybiel’s group observed that CalDAG-GEFI was exceptionally plentiful in the main compartment of the brain’s striatum in the late 1990s, it piqued their curiosity. CalDAG-effects GEFI’s on behavior was unknown for a long time, despite the fact that their study found the protein to be critical for regulating movement and even uncovering an essential part in blood clotting. It’s satisfying, according to Graybiel, that this long-standing curiosity has finally resulted in the discovery of a prospective therapy method for drug misuse disorder. As part of the McGovern Institute’s new addiction effort, her group will continue to investigate the molecular processes that underpin addiction.